The stethoscope is a medical instrument that allows you to perceive the sounds emitted by the heart, lungs and bowels. The procedure is referred to as "auscultation" and is typically performed by a physician or trained healthcare professional. However, you too can learn how to use one; Read on to learn more.
Steps
Part 1 of 7: Choosing and Adjusting the Stethoscope

Step 1. Purchase a high quality tool
This is a fundamental detail, because the better the stethoscope, the easier it will be to perceive the sounds emitted by the patient's body.
- Single-tube models are better than double-tube models, as these can come into contact with each other and create a rustle that hides the sounds of the heart.
- An instrument with a short, thick, relatively stiff tube is definitely more efficient, unless you want to keep it around your neck. In this second case you should choose a stethoscope with the longer tube.
- Make sure there are no leaks by tapping on the diaphragm (the flat part of the bell) and listening to the sound from the earphones. If you don't feel anything, there may be a leak.

Step 2. Adjust the earphones
You have to be sure that these elements are facing forward and that they fit well in your ears; otherwise you will not be able to perceive any sound.
- Make sure the earbuds are facing forward. If they were in the opposite direction, you wouldn't hear anything.
- Also check that they fit well in your ears and that they "seal" the ear canal to prevent ambient noise from passing through. If you find that they are not suitable for your anatomical shape, remember that most stethoscopes have removable and interchangeable toggles (the end of the earpiece). Go to a medical supply store and purchase different accessories.
- Some stethoscopes are constructed in such a way that the toggles can be tilted forward to ensure a good fit.

Step 3. Check the earband tension
In other words, make sure the toggles are close to your head, but not too tight. If they are too loose or too tight, change their position.
- If the earbuds are too wide, you won't be able to hear anything. To tighten them, just squeeze the toggles.
- If, on the other hand, they are too tight, then you may even feel pain and you will not be able to use the tool well. To release tension, gently spread the toggles apart.
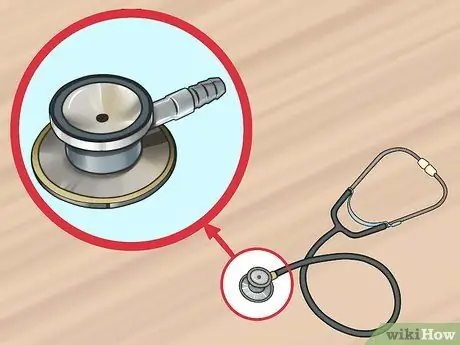
Step 4. Choose the suitable floating membrane
There are different types of "terminals" for the stethoscope and you must therefore purchase the one that best suits your needs. There are different sizes, for adults and children.
Part 2 of 7: Preparation

Step 1. Go to a quiet room to use the tool
Find a quiet area so that the sounds of the patient's body you want to hear will not be overwhelmed by background noise.

Step 2. Ask the patient to get into position
To auscultate the heart and abdominal cavity, the subject must lie on his back. To hear the sounds of the lungs, however, you have to ask him to remain seated. In other words, make your patient comfortable. The sounds of the heart, lungs and bowels are different according to the position assumed by the person (sitting, standing, lying on his side, and so on).
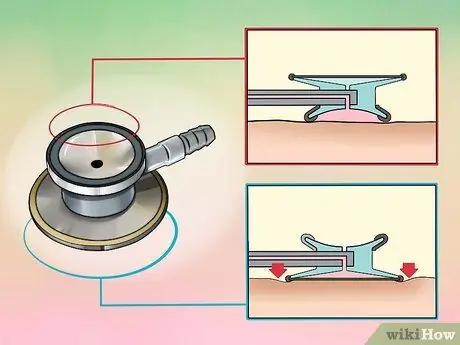
Step 3. Consider whether to use the bell or the diaphragm
The latter is the flat side of the floating membrane and lends itself to the auscultation of high and medium frequency sounds. The bell, the round side of the floating membrane, allows you to perceive low frequency sounds.
If you want an instrument with truly excellent acoustic qualities, then you must evaluate the electronic stethoscope: it is equipped with an amplifier that allows you to hear the heart and lungs without any difficulty; keep in mind, however, that this great ease of use and efficiency is accompanied by a very high cost

Step 4. Ask the patient to put on a hospital gown or pull up their clothes to expose bare skin
This step is essential to avoid the rustling generated by the fabric. If the patient is a man with a lot of chest hair, hold the stethoscope as still as possible to avoid the noises generated by the hair.
Warm the terminal of the stethoscope by rubbing it on a sleeve or buy a specific warmer, so that the patient does not feel discomfort in contact with the metal
Part 3 of 7: Auscultate the Heart

Step 1. Place the diaphragm over the patient's heart
The exact point is the upper left chest, where the fourth and sixth ribs join, just below the breast. Grab the tool between your index and middle fingers, applying light pressure, just enough to not hear your fingers rubbing together.

Step 2. Listen for the heartbeat for a full minute
Ask the patient to relax and breathe normally. You should hear normal human heart sounds that resemble "tum-da". These correspond to the systolic and diastolic phase; when you hear a "tum" you are listening to the systolic phase of the heart, while the "da" indicates the diastolic phase.
- The systolic "tum" sound is heard when the mitral and tricuspid valves close.
- The diastolic "da" sound is heard when the aortic and pulmonary valves close.

Step 3. Count the number of beats in one minute
The resting heart rate for adults and children over 10 years of age is between 60 and 100 beats per minute. In well-trained athletes this value drops to 40-60 beats per minute.
-
For children under 10, there are several normal ranges that vary with age:
- For newborns up to one month of age: 70-190 beats per minute;
- For infants from 1 to 11 months: 80-160 beats per minute;
- For children aged 1 to 2: 80-130 beats per minute;
- For 3-4 year olds: 80-120 beats per minute;
- Between 5 and 6 years of age: 75-115 beats per minute;
- For children aged 7 to 9: 70-110 beats per minute.

Use a Stethoscope Step 12 Step 4. Listen for abnormal heart sounds
As you count the beats, you should also pay attention to the presence of abnormal sounds. Anything that does not look like a "tum-da" is considered abnormal and the patient deserves further medical evaluation.
- If you hear a lapping or "tum … shhh … da" sound, the patient may have a heart murmur. This means that blood flows rapidly through the valves. Many people have what is called a physiological heart murmur. However, in some cases, this noise indicates heart valve problems and you should advise the patient to see a cardiologist when you hear the murmur.
- If you hear a third heart sound that resembles a low-frequency vibration, then the patient may have a ventricular defect. This third sound is called S3 or ventricular gallop. In this case, you must advise the patient to go to a cardiologist.
- Try listening to examples of normal and abnormal heart sounds to see if your patient has a normal heartbeat.
Part 4 of 7: Auscultate the Lungs

Use a Stethoscope Step 13 Step 1. Ask the patient to sit upright and breathe normally
As you proceed with the auscultation, you can ask him to take a deep breath if you don't hear anything or if the sounds are so soft that you don't notice any abnormalities.

Use a Stethoscope Step 14 Step 2. You need to use the stethoscope's diaphragm for this procedure
Listen to the noises emitted by the upper and lower lobes on both the patient's back and chest.
- While listening to the sounds, place the stethoscope on the upper part of the chest, then on the midclavicular line and finally on the lower part of the chest. Remember to analyze the front and back parts of each area.
- Compare both sides of the patient's lungs to each other for abnormalities.
- If you place the stethoscope on all of these areas, you are sure to auscultate all the lung lobes.

Use a Stethoscope Step 15 Step 3. Listen for abnormal breath sounds
Normal breathing generates soft sounds, like blowing into a cup. Listen to examples of normal sounds to compare them with what you hear in your patient's chest.
-
There are two types of normal breath sounds:
- Bronchial: are those emitted by the passage of air in the tracheobronchial tree.
- Vesicular: they are generated by the passage of air over the lung tissues.

Use a Stethoscope Step 16 Step 4. Pay attention to abnormal sounds
These can be: hisses, crackles, hums and screeches. If you cannot hear any sound, then the patient may have air or fluid around the lungs, a thickening of the chest wall, decreased airflow, or lung hyperinflation.
-
There are four types of abnormal breath sounds:
- Wheezing: These are high-pitched sounds, particularly audible in the expiratory phase, although in some patients they also occur during inspiration. Many asthmatics have wheezing that can be heard even without a stethoscope.
- Stridors: they are loud, acute, rhythmic sounds very similar to hissing and which are perceived above all in the inhalation phase. They are caused by an obstruction in the back of the throat and can often be felt even without a stethoscope.
- Ronchi: they are similar to the noise of a person snoring. They cannot be perceived without a stethoscope and occur because air has to follow an "irregular" path through the lungs or overcome obstructions.
- Crepitii: they are popping sounds, similar to the rales that are heard in the lungs. They are perceived in the inhalation phase.
Part 5 of 7: Listening to the Abdominal Sounds

Use a Stethoscope Step 17 Step 1. Place the diaphragm on the patient's bare abdomen
Use the subject's navel as a central point of reference and divide the abdomen into four auscultation zones. Start from the top left section, then top right, then bottom left, and finally bottom right.

Use a Stethoscope Step 18 Step 2. Listen for normal bowel noises
They are very similar to when the stomach "rumbles" with hunger. Any sound other than this could indicate an abnormality and the patient should be evaluated further.
You should hear a gurgle in all four sections. Sometimes, after surgery, it takes some time for the bowels to make noises again

Use a Stethoscope Step 19 Step 3. Pay attention to abnormal noises
Most of the sounds you can hear while listening to a person's abdomen are generated by digestion. Although, in most cases, they are completely normal, abnormal sounds could indicate a problem. If you are concerned that what you are hearing is not physiological, or the patient is showing a number of other symptoms, then you should refer him to a gastroenterologist.
- If you don't hear any noise, then there may be an obstruction in the stomach. Another cause could be constipation and the sounds could recur on their own after a short time. However, if the abdomen does not make sounds again, then there may be a blockage; in this case the patient needs further investigations.
- If you can hear a lot of noises followed by absolute silence, then there may be a breakdown or necrosis of the visceral tissue.
- If the patient has very high frequency sounds, then he may be suffering from an intestinal obstruction.
- Slow sounds can be caused by drugs, spinal anesthesia, infections, trauma, abdominal surgery, or abdominal hyperextension.
- Rapid noises that indicate intestinal hyperactivity can be caused by Crohn's disease, gastrointestinal bleeding, food allergies, diarrhea, infection, or ulcerative colitis.
Part 6 of 7: Auscultate the Vascular Murmur

Use a Stethoscope Step 20 Step 1. Assess whether vascular murmur needs to be checked
If you have noticed a sound that resembles a heart murmur, then you should investigate further. Since heart murmur and vascular murmur are similar, it's important to look for both when you hear the sound of either.

Use a Stethoscope Step 21 Step 2. Place the diaphragm of the stethoscope over one of the carotid arteries
They are located in the front of the neck, on the sides of the Adam's apple. If you slide your index and middle fingers along the throat, from top to bottom, you trace the course of the two carotids.
Do not press too hard on the arteries, as this could cut off the blood flow to the brain and cause the person to pass out. Never press both carotids at the same time

Use a Stethoscope Step 22 Step 3. Listen for the vascular murmur
This is a swash that indicates narrowing of the artery. It is sometimes confused with heart murmur because it is very similar, but the vascular murmur is stronger when heard in the carotid arteries than when heard in the heart.
Part 7 of 7: Check Blood Pressure

Use a Stethoscope Step 23 Step 1. Wrap the cuff around the patient's arm, just above the elbow
If the subject is wearing long-sleeved clothes, ask him to tuck them up. Make sure the cuff is the right size for the patient's arm; it must fit well without over-tightening. If this item is too small or too large, change it to one of the correct size.

Use a Stethoscope Step 24 Step 2. Place the stethoscope diaphragm on the brachial artery, just below the edge of the cuff
You could also use the bell, but with the diaphragm you can better perceive sounds. You need to hear Korotkoff sounds, which are pulsating, low-frequency noises that indicate systolic pressure.
Look for pulsations on the inside of your elbow to better understand where your patient's brachial artery is

Use a Stethoscope Step 25 Step 3. Inflate the cuff up to 180 mmHg or up to 30 mmHg beyond the systolic value you expect
You can detect these values by looking at the pressure gauge located on the sleeve. Next you need to let the air out of the cuff itself at a moderate rate (3 mmHg per second). As you do this, pay attention to the sounds in the stethoscope and observe the sphygmomanometer (the pressure gauge on the cuff).

Use a Stethoscope Step 26 Step 4. Listen to the sounds of Korotkoff
The first pulsing sound you can hear indicates the patient's systolic pressure. Note the pressure value indicated by the pressure gauge at this time. Subsequently, as you deflate the cuff, the sound stops and also in this case you have to write down the pressure value. You found your diastolic blood pressure.

Use a Stethoscope Step 27 Step 5. Deflate the cuff completely and remove it
Once you have obtained the second pressure value, you can deflate and remove the cuff from the patient. At this point you should have two numbers indicating the patient's pressure; write them next to each other separated by a diagonal bar (for example 110/70).

Use a Stethoscope Step 28 Step 6. If you want to do a second detection, wait a few minutes
If the readings are high, you will need to measure your blood pressure again.
If the systolic pressure is above 120 and the diastolic above 80, then the patient is hypertensive and must be examined by the doctor
Advice
Clean your instrument often. To avoid the spread of infections you should sanitize it after each use. You can use alcohol wipes or wipes and 70% isopropyl alcohol to make sure the stethoscope is disinfected
Warnings
- Do not immerse the stethoscope in water and do not expose it to very low or too high temperatures, in both cases you could damage the instrument.
- Don't talk and don't tap the bell while you have the earphones in your ears as it is very painful. You may even go so far as to damage your hearing based on how hard you tap or the volume of your voice.






